Acknowledgements & disclaimers
This Emergency Manual is in clinical use at the Alfred Hospital, in the context of the experience and processes in place there. This site and the information contained therein is provided by the authors to the wider health community as an educational resource only and is not intended to provide medical advice. It is not intended to be used to diagnose, treat, cure, or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice.
Practitioners must always rely on their own experience and knowledge in evaluating and using any information or methods described herein, being mindful of their own safety and the safety of others, including parties for which they have a professional responsibility. We do not accept any liability for any injury, loss or damage caused by use of the information provided in our website.
We make every effort to provide quality information in this site. However, we do not provide any guarantees, and assume no legal liability or responsibility for the accuracy, currency, or completeness of the information.
No data about consumers of this website is stored on our servers. This website uses necessary cookies to make the site work. These enable core security functionality. You may disable these by changing your browser settings, but this may affect how the website functions.
Acknowledgements & disclaimers
Contributors
Authors
- Julia Coull
- Maurice LeGuen
- Chris Nickson
- Sarah Yong
Web developer
Lloyd Roberts
The design of this manual was inspired by David Borshoff’s “The Anaesthetic Crisis Manual”
COVID ICU Crisis Preparedness Checklist
Check Cubicle Equipment
- Emergency Buzzer Location
- BVM Circuit + Viral Filter
- Chest Tube / Airway Clamp
- Hudson Mask (Tracheostomy Patients only)
- Prefilled Metaraminol Syringe
Assign Crisis Response Roles
- Medical Team Leader
- Nursing Team Leader
- Nursing 1st Responder (Fit face shield)
- Medical 1st Responder / Airway (Fit face shield)
- Checklist prompter / Scribe
- Runner
Top 10 tips for COVID-19 Crisis Management
- Fail to prepare, prepare to fail
- Safety first: there are no emergencies in a pandemic
- Call for help early
- Pre-allocate critical team roles
- The PPE spotter is there to save you from yourself
- Keep people in the room to a minimum
- Don face shield before entering room in any airway emergency
- Use clear, concise communication
- Reduce cognitive overload with checklists & aids
- Check that in-room equipment works before you need it
Communication in a Crisis
Principles of Communication in a Crisis (Use the 4C’s)
- Clear & Concise
- Cite Names
- Closed loop communication
(request, read back, confirm & update) - Cockpit Sterility
(maintain silence during critical procedures)
Encourage everyone to “speak up” whenever they have concerns using graded assertiveness (e.g. CUS approach)
- Concern
“I am concerned that the sats are falling” - Unsafe
“It is unsafe to continue intubation as the sats are less than 90%” - Stop
“Stop trying to intubate, we need to insert an LMA now”
- Brindley PG, Reynolds SF. Improving verbal communication in critical care medicine. Journal of Critical Care. 2011 Apr;26(2):155–9. FAA Pilot/ Controller Glossary. [Accessed 30 April 2020]. Available at URL: https://www.faa.gov/
air_traffic/ publications /media /pcg_4-03-14.pdf - Yamada NK, Halamek LP. Communication during resuscitation: Time for a change? Resuscitation. 2014 Dec;85(12):e191–2.
- Yamada NK, Halamek LP. On the Need for Precise, Concise Communication during Resuscitation: A Proposed Solution. The Journal of Pediatrics. 2015 Jan;166(1):184–7.
- Yamada NK, Fuerch JH, Halamek LP. Impact of Standardized Communication Techniques on Errors during Simulated Neonatal Resuscitation. Am J Perinatol. 2016 Mar;33(4):385–92.
Standardised Terms for use in a Crisis
| ABORT |
To terminate an action or procedure “Abort intubation, proceed with LMA insertion” |
| ACKNOWLEDGE |
Let me know that you have received & understood message “Administer 1mg IV adrenaline immediately”, “Acknowledge” |
| AFFIRM / AFFIRMATIVE |
Convey “yes”, confirmation or “correct” “Is oxygen connected?”, “Affirmative” |
| CANCEL |
Annul previous order “Cancel the normal saline bolus” |
| CONFIRM |
Request verification for information “Confirm SpO2 is >95%” |
| CORRECTION |
An error has been made in the message & the correct version follows “Increase propofol infusion to 20 mL/hr. Correction, increase propofol infusion to 15 mL/hr” |
| HOLD SHORT |
Stop before reaching the specified setting “Wean the noradrenaline but hold short of a MAP of 65 mmHg” |
| I SAY AGAIN |
Repeat for clarity or emphasis “”I say again: give 1 mg adrenaline IV immediately” |
| NEGATIVE |
Convey “No”, “Permission not granted” or “Not correct” “Is oxygen connect?”, “Negative, shall I connect oxygen now?” |
| READ BACK |
Repeat all, or the specified part, of my message exactly as received “Read back the adrenaline dose” |
| REQUEST |
I would like to know or wish to obtain “Request ABG result” |
| RESUME |
Resume a procedure or action that had been paused “Resume tracheal dilation” |
| STAND BY |
Wait until other action is completed then I will respond “Do you want normal saline or Hartmann’s?”, “Stand by” |
| SAY AGAIN |
Used to request a repeat of the last transmission “Say again all after step 2” |
| TIME |
To request time since resuscitation or procedure started “Time?”, “4 minutes since starting CPR” |
| UNABLE |
Inability to comply with an instruction or request “Please insert an arterial line”, “Arterial line unable” |
Critical Hypoxaemia in a Non-Intubated Patient
Bedside Staff
- Press Emergency Buzzer if SpO2 < 85% or if concerned
- Apply high flow oxygen at maximum rate (e.g. 15 L/min via face mask)
- Check oxygen connection & flow rate
- If patient arrests, perform compression only CPR
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Confirm high flow oxygen is being delivered
- Confirm SpO2 measurement accurate
- Obtain intubation trolley & prepare for intubation
- Assess patient for reversible causes
- Consider escalation of oxygen delivery strategy (e.g. HFNP, NIV, or intubation)
- Plan for intubation (if required) using COVID-19 intubation drop sheet & checklist
Critical Hypoxaemia in a Non-Intubated Patient
Recognition of Critical Hypoxaemia
Critical hypoxia is SpO2 <85% & requires emergency buzzer activation (unless modified SpO2 targets are documented by medical staff)
If critical hypoxia is not present, but the fraction of inspired oxygen (FiO2) to achieve target SpO2 range is increasing, bedside staff should notify ICU medical staff if:
- Oxygen flow has increased by an increment for >4 L/min since last medical review
- FiO2 has increased by >15% on HFNP or NIV
- Threshold limit of oxygen flow / FiO2 on current oxygen delivery device is reached,
- >4 L/min on nasal prongs
- >10 L/min on Hudson mask
- If concerned for any reason
Tips & Traps
Usual SpO2 targets are 92-96% for most patients & 88-92% in COPD patients who are CO2 retainers.
Consider common & lethal causes of hypoxaemia including:
|
|
If unsure of pulse oximetry accuracy, treat hypoxaemia & confirm with an arterial blood gas
Consider shunt if hypoxaemia dose not respond to increased FiO2
Critical Hypoxaemia in an Intubated Patient
Bedside Staff
- Press Emergency Buzzer if SpO2 < 85% or if concerned
- Increase FiO2 to 100%
- Assess the patient using the MASH approach
- Confirm ETCO2 waveform
- Connect BVM circuit (with viral filter) to wall oxygen at 15 L/min O2
- If patient arrests, perform compression only CPR
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Clamp ETT, turn off ventilator & disconnect from ventilator. Administer 15 L/min O2 via BVM circuit (with viral filter)
- Obtain ISBAR update from bedside nurse
- Confirm SpO2 measurement accurate
- Obtain intubation trolley & bronchoscope
- Assess for patient or ventilator causes using DOPES
Critical Hypoxaemia in an Intubated Patient
Recognition of Critical Hypoxaemia
Critical hypoxia is SpO2 <85% & requires emergency buzzer activation (unless modified SpO2 targets are documented by medical staff)
If critical hypoxia is not present, but the fraction of inspired oxygen (FiO2) to achieve target SpO2 range is increasing, bedside staff should notify ICU medical staff if:
- FiO2 has increased by >15% on HFNP or NIV
- Threshold limit of FiO2 is reached
- If concerned for any reason
Tips & Traps
Usual SpO2 targets are 92-96% for most patients & 88-92% in COPD patients who are CO2 retainers.
If unsure of pulse oximetry accuracy, treat hypoxaemia & confirm with an arterial blood gas
|
MASH Approach
|
DOPES
|
Consider common & lethal causes of hypoxaemia including:
|
|
Unplanned extubation
Bedside Staff
- Press Emergency Buzzer
- Increase ventilator FiO2 to 100%
- Check ETT position at teeth
- If clearly extubated:
- Turn off ventilator & cap ventilator tubing
- Apply high flow oxygen to face at maximum rate (e.g. 15 L/min)
- If patient arrests, perform compression only CPR
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Confirm ETCO2 waveform presence or absence
- Obtain intubation trolley & prepare for re-intubation
- Airway doctor takes control of airway
- If deteriorating SpO2 - 2-handed bag-mask ventilate
- If stable SpO2 - Do not squeeze bag
- Plan for re-intubation (if required) using COVID-19 intubation drop sheet & checklist
Unplanned extubation
Risk Factors for Inadvertent Extubation
|
Patient Factors
|
Staff Factors
|
Tips & Traps
Many patients (>50%) do not require reintubation if oxygenation & ventilation remain adequate
If stridor present or upper airway swelling suspected, a smaller ETT than previously used may be required
Prevention
- Ensure ETT is well secured
- Perform regular checks on ETT position and security
- Identify patients appropriate for Extubation as early as possible
- Ensure appropriate analgesia, sedation & delirium management plans are in place
- Additional staff should be provided during high risk procedures e.g. transport
- ICU consultant may consider use of mechanical constraints if deemed essential
- https://litfl.com/unplanned-extubation/
- Kiekkas P, Aretha D, Panteli E, Baltopoulos GI, Filos KS. Unplanned extubation in critically ill adults: clinical review. Nurs Crit Care. 2013 May;18(3):123-34. PMID: 23577947.
Unable to Ventilate / Ventilator Failure
Bedside Staff
- Press Emergency Buzzer
- Connect BVM circuit (with viral filter) to wall oxygen at 15 L/min O2
- If patient arrests, perform compression only CPR
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Turn off ventilator, Clamp ETT, Disconnect ventilator & cap tubing (leave ETCO2 & In-line suction connected to ETT)
- Connect BVM circuit (with viral filter) to patient (safe to bag patient if cuff is up)
- Obtain ISBAR update from bedside nurse
- Obtain intubation trolley
- Assess for patient or ventilator causes using DOPES
- Plan for re-intubation (if required) using COVID-19 intubation drop sheet & checklist
- Obtain new ventilator if required
Unable to Ventilate / Ventilator Failure
Recognition of Ventilation Emergency
DOPES – Will help to diagnose the problem
- Displacement of the ETT
- Obstruction of the ETT
- Patient – Pneumothorax, PE, Pulmonary oedema, Collapse
- Equipment malfunction
- ‘Stacked breaths’ – Bronchospasm
Tips & Traps
If BVM circuit ventilation is easy & patient improves:
- Equipment malfunction is likely to blame
- Check the ventilator circuit
- If there is nothing obviously wrong with the circuit – replace the ventilator
If BVM circuit ventilation is easy & patient does not improve:
- Suspect Displacement of the ETT or a circuit leak
If BVM circuit ventilation is difficult & patient does not improve:
- Minimal chest rise & fall → Suspect Obstruction of the ETT
- Check ETCO2 trace, attempt to pass in-line suction catheter
- Reasonable chest rise & fall → Patient factors are likely to blame
- Investigate systematically (see Critical Hypoxaemia in an Intubated Patient)
Tracheostomy Emergency: Respiratory Distress
Bedside Staff
- Press Emergency Buzzer
- Apply 100% oxygen to face & tracheostomy (Ventilator FiO2 100% & 15 L/min to face via Hudson mask)
- Attempt to pass in-line suction via tracheostomy
- If suction catheter does not pass or ETCO2 absent - Prepare occlusive dressing
- Connect BVM circuit (with viral filter) to wall oxygen
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Turn off ventilator - remove inner cannula
- Reconnect ventilator circuit & reattempt in-line suction
- If unsuccessful & ETCO2 still absent, deflate tracheostomy cuff & prepare to remove the tracheostomy
- Remove tracheostomy & cover with occlusive dressing
- Oxygenate from above using BVM circuit (with viral filter) (Do not bag unless SpO2 deteriorating)
- Plan for re-intubation using COVID-19 intubation drop sheet & checklist
Tracheostomy Emergency: Respiratory Distress
Tips & Traps
If a suction catheter cannot be passed the tracheostomy may be either blocked or dislodged.
- The inner cannula is designed as a safeguard in case of tracheostomy blockage with sputum – in an emergency the obstructed inner cannula can be removed
- Deflating the tracheostomy balloon may enable oxygenation from above in the case of complete tracheostomy obstruction or partial dislodgement
- A dislodged tracheostomy should be removed ASAP as it may be partially obstructing the airway or causing tissue distortion
Do not attempt to bag a potentially dislodged tracheostomy – This may result in rapid evolution of subcutaneous emphysema, leading to distortion of upper airway anatomy and potentially impairing ventilation.
If tracheostomy position is in doubt and patient can be oxygenated from above – a fiberoptic scope may be useful for confirming tube position & assessing obstruction
Reinsertion of a tracheostomy <7 days old is likely to be difficult and carries a high rate of complication – It is a relative contraindication if other options exist
Patient without a patent upper airway
- e.g. laryngectomy or obstructing pathology
- In these patients there is no option to oxygenate from above
- The focus should be on oxygenating through the neck
- A paediatric facemask can be used to create a seal (located in the tracheostomy emergencies draw of the intubation trolley)
Tracheostomy Emergency: Haemorrhage
Bedside Staff
- Press Emergency Buzzer
- Apply 100% oxygen via tracheostomy (Ventilator FiO2 100% or 15 L/min via trache shield if not ventilated)
- Attempt to clear airway using suction device
- Over inflate tracheostomy cuff with 20 mL air
- If patient arrests, perform compression only CPR
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
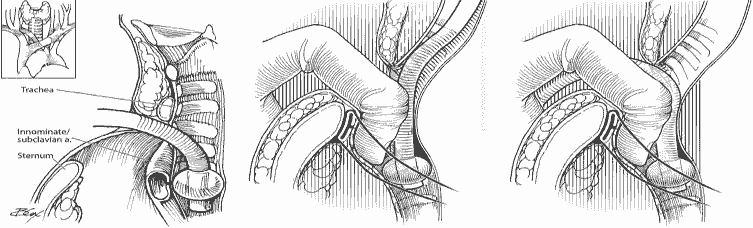
- If concern for tracheo-innominate fistula → Insert finger through stoma into pre-tracheal space to compress the innominate artery against posterior aspect of sternum
- Obtain intubation trolley & bronchoscopy tower
- Active Massive Transfusion Protocol
- Notify ENT Team & prepare for urgent OT transfer
- If ongoing bleeding consider bronchoscopy & reintubation
Tracheostomy Emergency: Haemorrhage
Causes of Trachostomy Haemorrhage
|
Early – Common, usually benign
|
Late – Uncommon, potentially life-threatening
|
Tracheo-innominate Fistula (TIF)
- TIF is a rare medical emergency
- Mortality rate is 100% without surgical intervention (25-30% of TIF patients who reach theatre survive)
- Hyperinflation of the tracheostomy cuff will temporarily control bleeding in 85% of cases
- Utley manoeuver can be attempted to control bleeding (described below)
Utley Manoeuvre
- Insert finger through stoma into pre-tracheal space to compress the innominate artery against the posterior aspect of the sternum
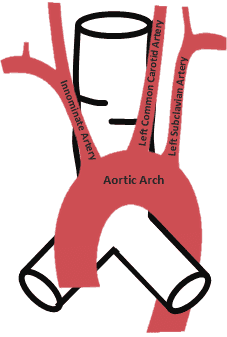
Innominate artery usually crosses the trachea at the 9th cartilage ring
- https://litfl.com/bleeding-tracheostomy/
- Pool, C & Goyal N. Operative management of catastrophic bleeding in the head and neck. Oper Tech Otolayngol Head Neck Surg. 2017 Dec;28(4):220-28.
Sudden Hypotension
Bedside Staff
- Press Emergency Buzzer if Systolic Blood Pressure <80 mmHg or MAP <55 mmHg
- Provide immediate BP management
- Give 250mL fluid bolus
- Increase Noradrenaline by 5 mcg/min or
- Prepare to give Metaraminol bolus - 0.5mg (1mL)
- Check ABCD-Equipment
- Place head of bed flat
- If patient arrests, perform compression only CPR
- Once first responders in room → move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Confirm ABCD-Equipment check, including accurate blood pressure measurement
- Ensure adequate IV access
- Assess for underlying cause of hypotension
Sudden Hypotension
Recognition of Critical Hypotension
Critical hypotension is SBP <80 mmHg or MAP < 55 mmHg & requires emergency buzzer activation (unless modified SBP targets are documented by medical staff)
If critical hypotension is not present, but the dose of vasoactive drug to achieve target MAP is increasing, bedside staff should notify ICU medical staff if:
- Noradrenaline / Adrenaline dose increased by 5 mcg/min
- Threshold limit of inotrope / vasopressor rate is reached
- If concerned for any reason
Tips & Traps
Usual MAP target is >65 mmHg for most patients, it may be altered in those with chronic hypertension or hypotension.
If unsure of arterial line accuracy, treat hypotension & confirm with a non-invasive blood pressure.
Check ABCD-Equipment
- Airway
- Breathing
- Circulation
- Drugs - correct, connected, infusing, not leaking
- Equipment and monitoring - BP transducer/cuff, ETT, ETCO2, SpO2
Underlying causes - is hypotension PROVED?
- Pump - cardiogenic?
- Rate - dysrhythmia?
- Obstruction - pneumothorax? pulmonary embolism? dynamic hyperinflation? abdominal compartment syndrome?
- Volume - bleeding? fluid loss?
- Endocrine - adrenal crisis? thyroid crisis? hypocalcaemia?
- Distributive - anaphylactic? septic? neurogenic? drugs?
- ? - errors in measurement or therapy
Cardiac Arrest
Bedside Staff
- Press Emergency Buzzer
- If not intubated - Apply 15 L/min O2 via Hudson mask & open patient’s airway
- If intubated - Increase ventilator FiO2 to 100%
- Perform compression only CPR
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in High Risk Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Continue with standard ACLS algorithm
- Avoid airway adjuncts & bag-mask ventilation
- Perform early intubation
Cardiac Arrest
DangerDroplet precautions |
Response |
Send for helpCode Blue (88) / emergency buzzer |
AirwayApply oxygen mask and open patient's airway Avoid oropharyngeal airways and bag-valve-mask |
BreathingBreathing assessed by looking (do NOT listen or feel) |
CPRCompressions only |
DefibrillateDefibrillate at a distance (from foot of bed) Stop oxygen flow but leave mask on patient Re-start oxygen flow when compressions start |
Early Intubation*Perform only after airborne precautions Use video laryngoscopy (if available) Early discussion of goals |
|
*A supraglottic airway device (SAD) is an acceptable alternative to intubation if:
|
Major Haemorrhage
Bedside Staff
- Press Emergency Buzzer
- If appropriate → Apply direct pressure to bleeding point
- Identify rapid IV access point
- If patient arrests, perform compression only CPR
- Once first responders in room → leave room to decontaminate if required
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Activate Massive Transfusion Protocol (#63100)
- Request: 4u PRBC, 2u FFP, 1u Platelets
- Complete & send release card via Spotless Staff
- Alternate Blood Bank Number #63016
- Take baseline bloods - ABG / FBC / Coags
- Allocate Blood checkers × 2
- Enter room in High Risk Airborne + Contact PPE
- Order form signed out of room after doffing of PPE
- Early contact to relevant surgical team
Major Haemorrhage
Major Haemorrhage
- Loss of > one blood volume within 24 hours (~70 mL/kg)
- 50% of total blood volumes lost in < 3 hours
- Bleeding in excess of 150 mL/minute
Criteria for Activation of MTP
- Actual or anticipated 4 units PRBC in < 4 hours
- + haemodynamic instability
- +/- anticipated ongoing bleeding
- Severe thoracic, abdominal, pelvic or multiple long bone trauma
- Major obstetric, gastrointestinal or surgical bleeding
Tips & Tricks
- Consider Tranexamic Acid - Dose 1g IV
- Carefully monitor ionised Calcium level
- Use fluid warmer
- Monitor ABG / FBC / Coags every 30-60 minutes
- Consider Factor rVIIa in bleeding unresponsive to conventional therapy
Goals in Management of Massive Transfusion
| Parameters | Values to aim for |
| Temperature | > 35 °C |
| Acid-base status | pH >7.2, Base Excess <-6, Lactate <4 mmol/L |
| Ionised calcium | > 1.1 mmol/L |
| Haemoglobin | Should not be used alone as a transfusion trigger |
| Platelet | ≥50 × 109/L (> 100 × 109/L in TBI) |
| APTT | ≤1.5 × normal |
| Fibrinogen | ≥1.0 g/L |
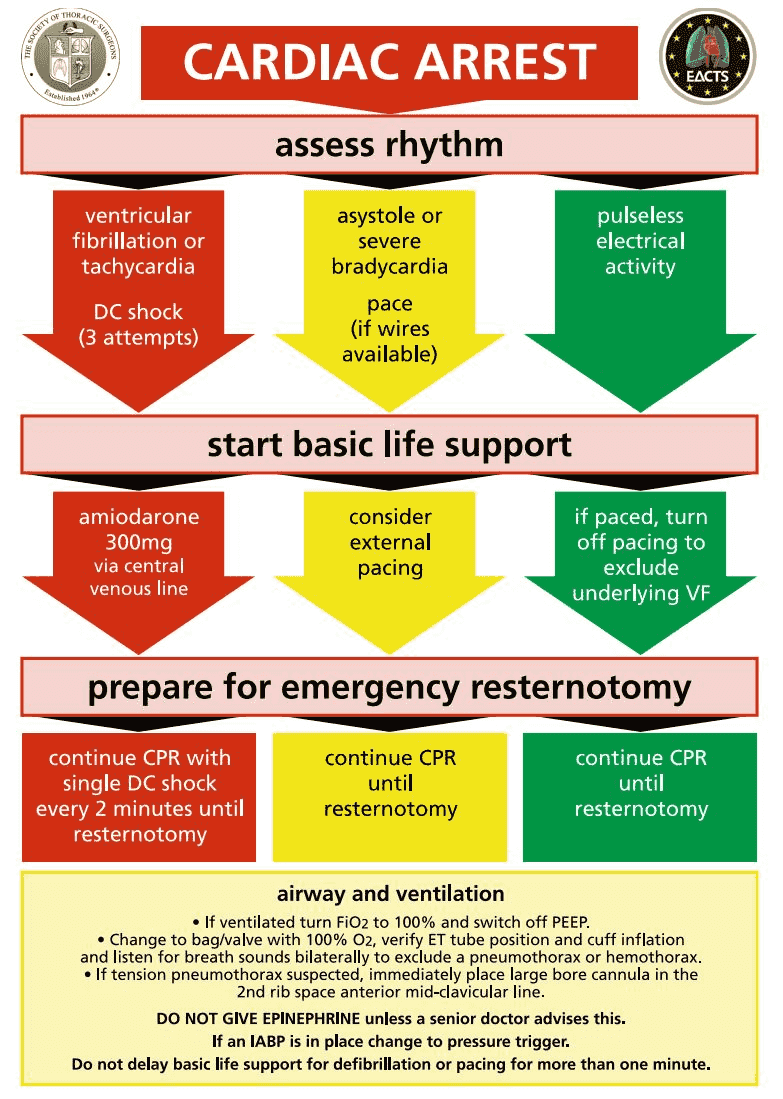
Cardiac Arrest In Post Cardiac Surgery Patient (Emergency Resternotomy)
Bedside Staff
- Press Emergency Buzzer
- If not intubated → Apply 15 L/min O2 via Husdon mask & open patient's airway
- If intubated → Increase ventilator FiO2 100%, PEEP to 0
- Assess rhythm
- PEA (Paced) → Pause to assess for VF
- Asystole → Emergency pace
- VT/VF → Defibrillate - 150J × 3
Delay CPR for up to 1 minute for above troubleshooting
- Perform compression only CPR
- Once first responders in room → move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Follow Post Cardiac Surgery ACLS algorithm
- Allocate Emergency Resternotomy Roles
- Perform early intubation (if required)
Cardiac Arrest In Post Cardiac Surgery Patient (Emergency Resternotomy)
Patient Agitation: Extubated Patient
Bedside Staff
- Press Emergency Buzzer
- Attempt verbal de-escalation
- Identify rapid IV access point
- Perform rapid ABCD assessment for immediately reversible causes
- Administer Haloperidol IV 2.5 mg
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Activate CODE GREY (if required) - Call 2222
- Establish IV access if required
- Document & communicate a BOC plan
- Use physical restraints if required for patient & staff safety
Patient Agitation: Extubated Patient
Immediately reversible causes of Delirium
- Hypoxia
- Hypoglycaemia
- Hypotension
- Drug withdrawal
Tips & Traps
Attempt verbal de-escalation techniques, including involving trusted others prior to chemical sedation
Non-pharmacological treatment options
- Recurrent orientation
- Early mobilisation and physiotherapy
- Early removal of catheters
- Day-night routine
- Sleep hygiene
- Involve family
- Noise control at night
Suggested sedation dosing
| Therapy | No IV access | IV access |
|---|---|---|
| 1st line | Olanzapine wafer 10 mg PO or Quetiapine 25 mg PO or Diazepam 10 mg PO |
Haloperidol or Droperidol 2.5 mg IV |
| 2nd line |
Haloperidol or Droperidol 5 - 10 mg IM |
Ketamine 1 mg/kg IV or Midazolam 2.5 mg IV |
| 3rd line | Ketamine 4 mg/kg IM | Consider intubation |
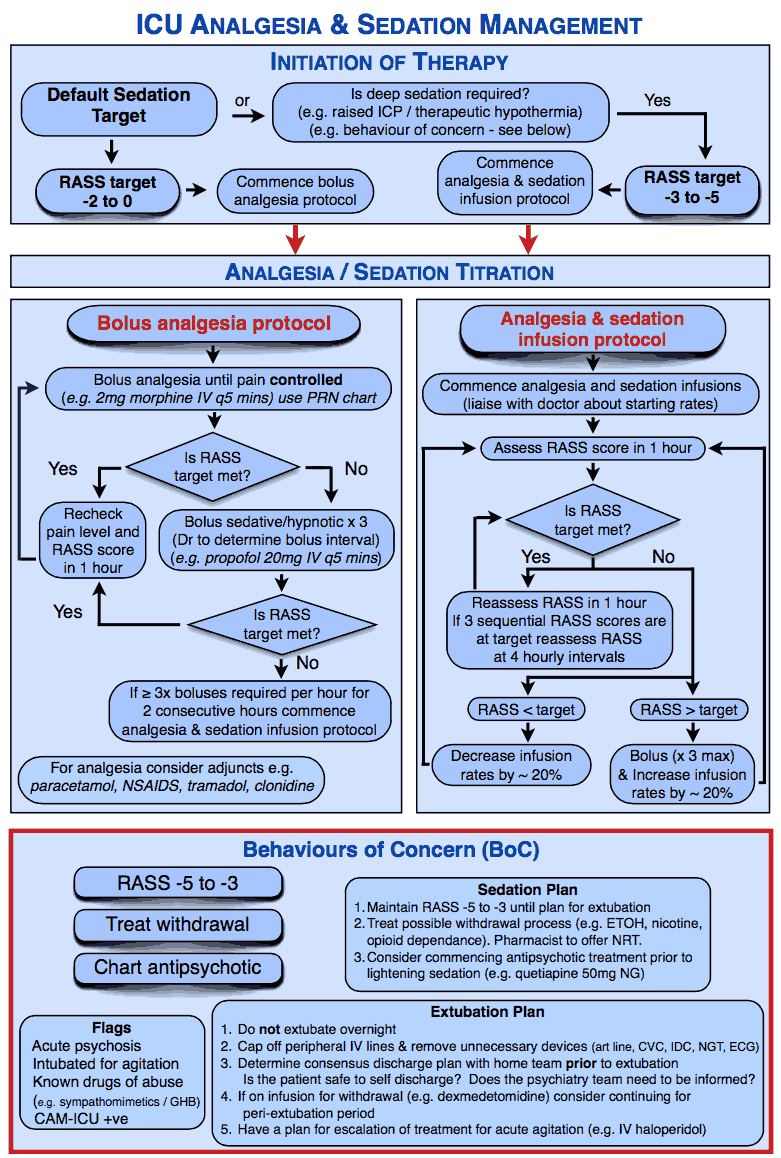
Patient Agitation: Intubated Patient
Bedside Staff
- Press Emergency Buzzer
- Bolus sedation
- Propofol 40mg (4mL)
- Midazolam 5mg
- Perform rapid ABCD assessment for immediately reversible causes
- Confirm ETT & central line positions unchanged
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Activate CODE GREY (if required) - Call 2222
- Establish IV access if required
- Document & communicate a BOC plan
- Use physical restraints if required for patient & staff safety
Patient Agitation: Intubated Patient
Seizure
Bedside Staff
- Press Emergency Buzzer
- Ensure patient safety - bed rails up, head protected
- If intubated - Bolus IV sedation
- Propofol 40mg or Midazolam 5mg
- If not intubated
- Apply 15 L/min O2 Husdon mask & open airway
- IV access - Midazolam 2.5mg IV or Clonazepam 1mg IV
- No IV access - Midazolam 10mg IM
- Once first responders in room - move away from head
Emergency Team
- Assemble team & confirm roles
- First responders, including Airway doctor, enter room in Airborne + Contact precautions
- Obtain ISBAR update from bedside nurse
- Activate CODE GREY (if required) - Call 2222
- Establish IV access if required
- Take baseline blood - ABG/FBC/UEC/CMP/LFT
- Obtain intubation trolley & prepare for intubation (if required)
- Consider differential diagnosis & anti-epileptic drug loading
Seizure
Common causes of seizures in ICU
|
Rapidly reversible |
Other |
|
|
Tips & Traps - Initial Treatment
|
Initial Treatment Phase |
Step 1: Benzodiazepine |
| 5-15 minutes |
|
|
Established status epilepticus |
Step 2: First line anti-epileptic drug (AED) (Choose one) |
| 15-30 minutes |
|